|
Related Science |
Saturated Fats and Heart Disease: The Clinical Trials
Some Facts:
- Dietary saturated fats increase blood cholesterol levels in feeding studies
- Replacing saturated fats with polyunsaturated fats decrease cholesterol levels
- The only 2 double-blind, randomized trials in history failed to show that a low-saturated fat diet decreases heart disease
- 3 meta-analyses published in the past 3 years concluded no decrease in heart disease associated with low saturated fat diet
Summary
In 1953, Ancel keys published the seminal 6-country ecologic study that found a striking correlation between total fat intake and cardiovascular mortality. It was based on his observations that increased meat consumption in America coincided with a rise in heart disease rates. This finding ignited the diet-heart hypothesis, linking dietary fat to cardiovascular disease.
Since the 1950s, there have been a relatively small number of large, long-term clinical trials examining the potential benefits of decreased saturated fats in the diet as a primary focus. All major trials since 1966 are listed in the bibliography below. Some took place in mental institutions, some were not randomized, and some also involved major confounding interventions such as weight loss, exercise, or increased fruit and vegetable consumption. Some show benefits to replacing saturated fats with polyunsaturated fats, while others do not.
If we were to focus on the largest (i.e. > 100 subjects), randomized, most famous trials ever done lasting longer than 1 year, we are left with very few to assess that meet the following 2 criteria:
1) The only significant intervention involved a reduction in fat and saturated fat and an increase in polyunsaturated fats
2) They ask the question: does this diet reduce heart disease? (defined as heart attacks or death from heart disease)
Listed in reverse chronological order:
Women’s Health initiative (2006) – 48,835 women, 8 years, no significant difference between intervention and control.
Diet and Reinfarction trial (1989) – 2,033 men, 2 years, no significant difference between the groups given and not given fat and fiber advice. No significant differences in ischaemic heart disease between intervention and control (intervention was only advice in this trial)
Minnesota Coronary Survey* (1989) – 4,393 men and 4,664 women, double-blind, 4 years, no significant reduction in cardiovascular events or total deaths from the treatment diet
Finnish Mental Hospital (1972) – 12 years, physicians not blinded, significant decrease in coronary heart disease (CHD)death in men ( 5.7 deaths /1000 person-years vs 13 deaths /1000 person-years in the control. Non-significant decrease in CHD in women. (Not randomized, although included here because this is main experiment cited in support of diet-heart hypothesis)
Los Angeles Veteran’s Trial* (1969) – 846 subjects, up to 8 years, non significant difference in primary endpoints – sudden cardiac death or myocardial infarction. More non-cardiac deaths in experimental group, resulting in near identical rates of total mortality
Oslo Heart Study (1968) – 412 men, 5 year, slight decrease in CHD with intervention. Many dietary interventions accompanied the low saturated fat diet. When stratified by age, the results were significant only in subjects younger than 60.
* Double blind
A full list of all the trials done supporting and refuting the saturated fat-heart-disease relationship, and a more in depth description of each, can be found in the bibliography section below. There are many others that did not meet the criteria I defined above.
Meta-analyses
If we instead focus on the recent meta-analyses of clinical trials testing this relationship, the majority have failed to elucidate a benefit associated with a low saturated fat diet:
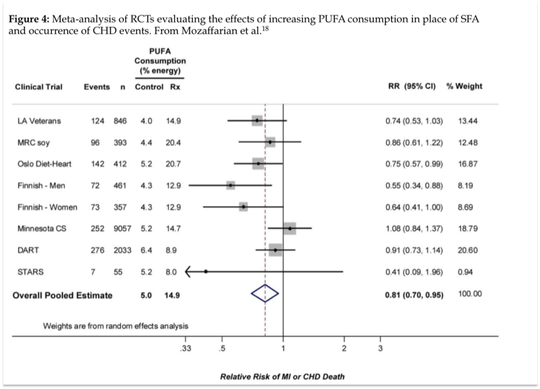
The only study above showing a benefit to replacing saturated fats with polyunsaturated fats was the Mozaffarian meta-analysis. The authors of the study claim to have only included randomized clinical trials in their meta-analysis. Surprisingly, the Finnish Mental Hospital Study was included twice – split into separate analytical pools of male and female subjects. It is unclear why this study was even included to begin with, since it was not randomized and contained a disproportionate number of control subjects who were taking cardio-toxic medications and consuming higher levels of trans fats than the experimental group (see Miettinen et al below).
Inclusion of male and female Finnish data separately further raises concern since it clearly exaggerates the apparent cardio-protective effect of PUFAs demonstrated in this meta-analysis. Excluding the Finnish data from their pooled analysis would diminish the observed results and elicit a null finding, since all other included studies apart from the Oslo heart study (RR=0.75, CI 0.57-0.99) were null:
Since the 1950s, there have been a relatively small number of large, long-term clinical trials examining the potential benefits of decreased saturated fats in the diet as a primary focus. All major trials since 1966 are listed in the bibliography below. Some took place in mental institutions, some were not randomized, and some also involved major confounding interventions such as weight loss, exercise, or increased fruit and vegetable consumption. Some show benefits to replacing saturated fats with polyunsaturated fats, while others do not.
If we were to focus on the largest (i.e. > 100 subjects), randomized, most famous trials ever done lasting longer than 1 year, we are left with very few to assess that meet the following 2 criteria:
1) The only significant intervention involved a reduction in fat and saturated fat and an increase in polyunsaturated fats
2) They ask the question: does this diet reduce heart disease? (defined as heart attacks or death from heart disease)
Listed in reverse chronological order:
Women’s Health initiative (2006) – 48,835 women, 8 years, no significant difference between intervention and control.
Diet and Reinfarction trial (1989) – 2,033 men, 2 years, no significant difference between the groups given and not given fat and fiber advice. No significant differences in ischaemic heart disease between intervention and control (intervention was only advice in this trial)
Minnesota Coronary Survey* (1989) – 4,393 men and 4,664 women, double-blind, 4 years, no significant reduction in cardiovascular events or total deaths from the treatment diet
Finnish Mental Hospital (1972) – 12 years, physicians not blinded, significant decrease in coronary heart disease (CHD)death in men ( 5.7 deaths /1000 person-years vs 13 deaths /1000 person-years in the control. Non-significant decrease in CHD in women. (Not randomized, although included here because this is main experiment cited in support of diet-heart hypothesis)
Los Angeles Veteran’s Trial* (1969) – 846 subjects, up to 8 years, non significant difference in primary endpoints – sudden cardiac death or myocardial infarction. More non-cardiac deaths in experimental group, resulting in near identical rates of total mortality
Oslo Heart Study (1968) – 412 men, 5 year, slight decrease in CHD with intervention. Many dietary interventions accompanied the low saturated fat diet. When stratified by age, the results were significant only in subjects younger than 60.
* Double blind
A full list of all the trials done supporting and refuting the saturated fat-heart-disease relationship, and a more in depth description of each, can be found in the bibliography section below. There are many others that did not meet the criteria I defined above.
Meta-analyses
If we instead focus on the recent meta-analyses of clinical trials testing this relationship, the majority have failed to elucidate a benefit associated with a low saturated fat diet:
- In 2010, Ramsden et al. published a meta-analysis of randomized clinical trials, including trials where polyunsaturated fats (PUFAs) were increased in place of saturated fats (SFAs) and/or trans fatty acids (TFA), and non-fatal heart attacks, Coronary heart disease-related deaths, and/or total deaths were reported. In the nine studies included, there was a non-significant increased pooled risk of 13% for n-6 PUFA intake (RR=1.13, CI: 0.84, 1.53) and a decreased risk of 22% (RR=0.78, CI: 0.65, 0.93) for mixed n-3/n-6 PUFA diets. In other words, increasing polyunsaturated fats in the diet provides no benefit, and may be harmful according to this study.
- Also in 2010, Mozaffarian et al published a systematic review and meta-analysis of randomized clinical trials investigating the effects of increasing PUFAs in place of other nutrients. Among the seven studies included, an overall pooled risk reduction of 19% (RR= 0.81, CI=0.83-0.97) was observed for each 5% of energy of increased PUFA in the diet.
- In 2009, Mente et al. published a systematic review of the randomized clinical trial (RCT) evidence that supports a causal link between various dietary factors and coronary heart disease The pooled analysis from 43 RCTs showed that increased consumption of marine omega-3 fatty acids (RR=0.77; 95% CI: 0.62-0.91) and a Mediterranean diet pattern (RR=0.32, 95% CI: 0.15-0.48) were each associated with a significantly lower risk of CHD. Higher intake of polyunsaturated fatty acids or total fats were not significantly associated with CHD, and the link between saturated fats and CHD received a Bradford Hill score of only 2 (out of a maximum score of 4), signifying weak evidence of a causal relationship.
- Also in 2009, the Cochrane Collaboration, an international not-for-profit organization, published a meta-analysis of clinical trials that either reduced or modified dietary fat for preventing cardiovascular disease. Twenty-seven studies met the inclusion criteria, and no significant effect on total mortality (RR = 0.98, 95% CI: 0.86-1.12) or cardiovascular mortality (RR = 0.91, 95% CI: 0.77-1.07) was found between the intervention and control groups
The only study above showing a benefit to replacing saturated fats with polyunsaturated fats was the Mozaffarian meta-analysis. The authors of the study claim to have only included randomized clinical trials in their meta-analysis. Surprisingly, the Finnish Mental Hospital Study was included twice – split into separate analytical pools of male and female subjects. It is unclear why this study was even included to begin with, since it was not randomized and contained a disproportionate number of control subjects who were taking cardio-toxic medications and consuming higher levels of trans fats than the experimental group (see Miettinen et al below).
Inclusion of male and female Finnish data separately further raises concern since it clearly exaggerates the apparent cardio-protective effect of PUFAs demonstrated in this meta-analysis. Excluding the Finnish data from their pooled analysis would diminish the observed results and elicit a null finding, since all other included studies apart from the Oslo heart study (RR=0.75, CI 0.57-0.99) were null:
The evidence from clinical trials fails to show that the simple act of replacing SFAs with PUFAs decreases the risk of CHD. The only two randomized, double blind trials ever performed - the Minnesota Coronary Survey and the Los Angeles Veterans Trial - both taking place in highly controlled feeding environments and lasting 4.5 and 8.5 years respectively, failed to show a reduction in CHD risk or total mortality. Some may argue that the Los Angeles Veterans study did show a benefit, yet this only reached significance upon inclusion of secondary endpoints, such as cerebral infarction, ruptured aneurysms, and limb amputations due to peripheral artery disease. The Finnish mental study showed a benefit in men, however the study design and uneven distribution of cardiotoxic medications warrants careful interpretation of the findings and likely diminishes the external validity of these observations. The only randomized dietary trials performed in free-living individuals that have been successful in reducing CHD risk – the Lyon heart study and Oslo diet-heart trial – did so with a comprehensive dietary intervention approach that manipulated so many aspects of the diet that the independent role of dietary fatty acids cannot be ascertained.
Bibliography
Jump to a section:
Meta-analyses and reviews showing no benefit to low saturated fat diet
Clinical trials showing no decrease in heart disease associated with low saturated fat diet
Meta-analyses and reviews showing a decrease in heart disease associated with a low saturated fat diet
Clinical trials showing a decrease in heart disease associated with low saturated fat diet
Ramsden et al. (2010). n-6 Fatty acid-specific and mixed polyunsaturate dietary interventions have different effects on CHD risk: a meta-analysis of randomised controlled trials
Outcome: In the nine studies included, there was a non-significant increased pooled risk for non-fatal myocardial infarctions (MI) and coronary heart disease (CHD) death of 13% for n-6 Poly unsaturated fats (PUFA) intake (RR=1.13, CI: 0.84, 1.53) and a decreased risk of 22% (RR=0.78, CI: 0.65, 0.93) for mixed n-3/n-6 PUFA diets as compared to the control groups.
- Overview: Studies were included if PUFA were increased in place of saturated fats (SFA) and/or Trans fats (TFA) and non-fatal MI, CHD deaths and/or total deaths were reported.
The Cochrane Collaboration (2009). Reduced or modified dietary fat for preventing cardiovascular disease
Outcome: 27 studies included (40 intervention arms, 30,901 person-years). There was no significant effect on total mortality (rate ratio 0.98, 95% CI 0.86 to 1.12) or cardiovascular mortality (rate ratio 0.91, 95% CI 0.77 to 1.07), and slightly significant protection from cardiovascular events (rate ratio 0.84, 95% CI 0.72 to 0.99), which became non-significant during sensitivity analysis.
- Overview: A meta-analysis assessing the effect of reduction or modification of dietary fats on total and cardiovascular mortality and cardiovascular morbitity over at least 6 months, using all available randomized clinical trials that fulfilled the following criteria: 1) randomized with appropriate control, 2) intention to reduce or modify fat or cholesterol intake (excluding omega-3 interventions), 4) not multi factorial, 5) intervention at-least 6-months, 6) mortality and cardiovascular morbidity data available.
- Comments: Cochrane collaboration is one of the most well-respected non-profit organizations created to provide non-bias systematic analyses. Trials that lasted longer than 2 years showed significant reductions in the rate of cardiovascular events, and a non-significant suggestion of total mortality protection. They concluded by saying: “It is not clear whether a low fat diet, a modified fat diet, or a combination of both is most protective of cardiovascular events.”
Mente et al. (2009). A Systematic Review of the Evidence Supporting a Causal Link Between Dietary Factors and Coronary Heart Disease
Outcome: The pooled analysis from 43 RCTs showed that increased consumption of marine omega-3 fatty acids (RR=0.77; 95% CI: 0.62-0.91) and a Mediterranean diet pattern (RR=0.32, 95% CI: 0.15-0.48) were each associated with a significantly lower risk of CHD. Higher intake of polyunsaturated fatty acids or lower intake of total fats was not significantly associated with CHD. Specifically the evidence for the association between saturated fats and CHD received a Bradford Hill score of only 2 (out of a maximum score of 4), signifying weak evidence of a causal relationship.
Howard et al. (2006). Low-fat dietary pattern and risk of cardiovascular disease: The women’s health initiative randomized controlled dietary modification trial
Outcome: After 8 years, the diet had no significant effect on incidence of cardiovascular disease in the 48,835 women enrolled. At year 6, mean fat intake decreased by 8.2% as compared to the control group, with a 2.9% decrease in saturated fat; LDL and systolic BP decreased by 3.55 mg/dl, and 0.31 mg hg respectively.
- Overview: Randomized intervention trial of 48,835 post-menopausal women for a mean of 8.1 years. 40% randomized to intervention and 60% randomized to control.
- Intervention: The Intervention group received both group and individual sessions to promote a decrease in fat intake to 20% of calories, and increase vegetable, fruit, and grain consumption(to 6+ servings per day). Did not include weight loss or caloric restriction goals. The Control group received diet-related education material
- Comments: One of the largest dietary clinical trials ever. Diet assessed by Food Frequency Questionnaires, not food records or dietary recall. Intervention group significantly lowered their total fat intake (although not below 20%). At year one, 8% of calories were coming from saturated fat, while at year 6, mean intake was 9.5% of calories. There were also significantly increases in fiber, vegetables, fruits, total grains, and whole grains. Researchers concluded that “over a mean of 8.1 years, [this] dietary intervention…did not significantly reduce the risk of CHD, strong, or CVD in postmenopausal women, and achieved only modest effects on CVD risk factors.”
Burr et al (1989). Effects of changes in fat, fish, and fibre intakes on death and myocardial reinfarction: Diet And Reinfarction Trial (DART)
Outcome: No significant difference between the groups given and not given fat and fiber advice. Total mortality was significantly lower in the fish advice group, than the no fish advice group. No significant differences in ischaemic heart disease (IHD) events between fish advice and no fish advice groups (more non-fatal infarctions occurred in the fish advice group)
- Overview: 2 year, randomized trial in 2,033 men 70 years old or younger examining effects of fat, fiber, and fish intake on heart disease.
- Main Points: Randomized to 1 of 3 groups which would receive differing advice: Group 1. reduce fat to 30% of total energy and increase polyunsaturated/saturated ratio to 1.0, Group 2. advised to eat 2 weekly portions of fatty fish, and Group 3: increase cereal fiber intake to 18 grams daily.
- Comments: Hardly any difference in fat intake between the fat advice and no advice groups. Only intervention which seemed to have any effect was increase in fatty fish intake, which decreased mortality but not infarctions.
Frantz et al (1989). Test of effect of lipid lowering by diet on cardiovascular risk. The Minnesota Coronary Survey
Outcome: After 4.5 years, no reduction in cardiovascular events or total deaths from the treatment diet, with a non-significant trend towards a benefit to a high saturated fat diet. Results observed despite a 14.5% reduction in cholesterol levels in the experimental group.
- Overview: 4.5 year, double-blind, randomized trial in 6 Minnesota state mental hospitals and one nursing home involving 4,393 men and 4,664 women, examining effects of a lipid lowering diet on heart disease.
- Main Points: Intervention: 38% fat diet (9% Saturated fat, 15% polyunsaturated fat, 14% monounsaturated, 166 mg cholesterol); Control diet: 39% fat diet (18% saturated fat, 5% polyunsaturated fat, 16% monounsaturated fat, 446mg cholesterol) Intervention group cholesterol levels decreased 14.5% and were stable for the entire study. Control and intervention foods were indistinguishable from each other.
- Comments: Rare double blind dietary clinical trial. Average total time in hospital for each subject was 384 days. The number of person years observed was 9,538, with 5,903 of these years continuously for more than 2 years and 2,495 for more than 4 years. Cholesterol diet did not seem to be effective, although average hospital stay was only 1 year.
MRFIT Research Group (1982). Multiple Risk Factor Intervention Trial (MRFIT)
Outcome: After 7 years, mortality from CHD was 17.9 deaths per 1,000 in the intervention group, and 19.3 per 1,000 in the control group, a non-significant difference of 7%. Total mortality rates were 41.2 per 1,000 in the intevention group and 40.4 per 1,000 in the control group, also not significantly different.
- Overview: Randomized primary prevention trial testing effects of multi-factor intervention on mortality from coronary heart disease (CHD) in 12,866 high-risk men aged 35-57, in which men were randomized to either the special intervention (SI) or the usual care (UC) for a mean time of seven years
- Main Points: The Special intervention (SI) consisted of: stepped-care treatment of hypertension, counseling for cigarette smoking, and dietary advice for lowering blood cholesterol levels. The dietary advice consisted of: reducing saturated fat intake to less than 10% of calories (later changed to <8%), dietary cholesterol intake < 300mg (later changed to < 250mg). Usual care (UC) consisted of their usual source of healthcare in their community.
- Comments: One of the largest clinical trials ever examining dietary interventions and CHD. There were 2 other major co-contaminant interventions — hypertension treatment and smoking cessation. After 2 years on the cholesterol lowering diet blood cholesterol in the SI and UC groups decreased by 10 mg/dL and 3.4 mg/dL respectively. After 6 years, the mean levels were reduced by 12.1 mg/dL and 7.5 mg/dL. This decrease was 50% less than the researchers hoped for. However, with blood pressure medications, smoking cessation counseling, and a decrease in blood cholesterol levels, it is surprising that there were no significant CHD differences between the groups.
Dayton et al (1969). A controlled trial of a diet high in unsaturated fat (Los Angeles VA Trial)
Outcome: After 8 years of this double-blind feeding study, there was no difference in primary endpoints - sudden death or myocardial infarction between the control and experimental groups. When pooled with the data for cerebral infarction and other secondary end points likely unrelated to diet, such as extremity amputation due to peripheral vascular disease, the totals were 96 in the control group and 66 in the experimental group; P=0.01. However, deaths due to nonatherosclerotic causes were higher in the experimental group (85 vs 71 in control), resulting in near identical rates of overall mortality.
- Overview: Double blind, randomized trial involving 846 subjects for up to 8 years. Subjects lived in a domilicary unit and were former veterans. Half ate a control diet, similar to the american diet, and half ate the experimental diet. All meals served in cafeteria.
- Main Points: Subjects given meal tickets of a certain color, corresponding to a particular diet unknown to the subjects. The control diet was 40% calories from fat, “mostly of animal origin.” The experimental diet involved substitution of vegetable oils for 2/3 of the animal fat, incorporated into the diet in form of milk, ice cream, margarine, and cheeses. Serum cholesterol averaged 13% lower in the experimental group.
- Comments: This is one of the most famous studies cited in support of the diet-heart hypothesis. It can arguably be categorized as beneficial or not, depending on which outcomes you choose. However, since there was a non-significant difference in the primary endpoints – myocardial infarction of sudden cardiac death, it was categorized as not beneficial. It also raised an interesting question as to whether or not a diet high in unsaturated fat may contribute to death by other causes, since the experimental group had more non-cardiac deaths (specifically from cancer: 7 deaths in experimental, and 2 in control). This was not confirmed in other major clinical trials however.
Rose et al (1965). Corn oil in treatment of ischaemic heart disease.
Outcome: At 2 years, the proportion of patients remaining free of major cardiac events was greater in control group (75%) as opposed to the olive oil group (57%) or the corn oil group (52%), which was close to significance, but not significant.
- Overview: Randomized 2 year clinical trial (3 years were planned, but half subjects lost to death, re-infarction or lost to follow-up) to study effects of vegetable oil on heart disease. 80 subjects enrolled, with previous myocardial infarction (MI) or clear history of angina, under 70 years old, without heart failure.
- Main Points: Subjects randomized to control group, olive oil group, or corn oil group. Physicians were not blinded to which subjects were taking oil, however they did not know which oil each intervention group subject was taking. The intervention diet group was: told to limit fried foods, fatty meats, ice cream, milk, eggs, butter. An oil supplement of 80g/day was taken at each meal
- Comments: Dietary assessment taken during second year of follow up with a questionnaire. Researchers estimated that during the first year about 90% of subjects took their pills, while only 60% took it during the second year. Researchers concluded saying: “corn oil cannot be recommended as a treatment for ischaemic heart disease It is most unlikely to be beneficial, and it is possibly harmful.”
Mozafarrian et al (2010). Effects on coronary heart disease of increasing polyunsaturated fat in place of saturated fat: A systematic review and meta-analysis of randomizd controlled trials.
Outcome: Overall pooled risk reduction was 19% (RR=0.81, 95% CI 0.70 to 0.95, p=0.0008), corresponding to a 10% reduced CHD risk (RR=0.90, 95% CI 0.83-0.97) for each 5% energy increase of Polyunsaturated fats in place of saturated fats. This is the only recent meta-analysis to find a decrease in heart disease associated with a low saturated fat diet. Despite claiming they included only randomized trials, the Finnish mental study is included twice, divided into male and female data sets.
- Overview: Systematic review of the clinical trials investigating the effects of increased polyunsaturated fats, as a replacement of saturated fats, on cardiovascular heart disease (CHD) endpoints
- Main Points: Studies included if: randomized, increased consumption of Polyunsaturated fatty acids (PUFAs) for at least 1 year, without major co-contaminant interventions, had appropriate control group, and reported cardiovascular disease incidence. Out of 346 identified abstracts, only 8 trials met the criteria
- Comments: Replacing saturated fats with polyunsaturated fats may be beneficial for reducing heart disease. Long term trials showed greater benefits, “suggesting that benefits of increasing PUFA consumption accrue over time.” However, this conclusion is very misleading given the fact that the only study showing a large protective effect included in this "meta-analysis of randomized trials" was a non-randomized trial. The data from this study, the Finnish mental study, was divided into male and female subgroups as separate data sets, further biasing the results.
Ornish et al (1998). Intensive lifestyle changes for reversal of coronary heart disease
Outcome: average % diameter stenosis at baseline decreased 1.75% after 1 year and 3.1% after 5 years. In control group, % diameter increased by 2.3% at 1 year and by 11.8% after 5 years. Chest pain frequency and duration were not different at 1 or 5 years. Chest pain severity was significantly decreased at 1 year in the experimental group, but not at 5 years.
- Overview: 1 year Randomized trial with 35 people assigned to a multi-factorial intensive lifestyle change, or no intervention, then extended for 4 more years.
- Intervention: The Experimental-group: asked to eat a low-fat vegetarian diet for at least a year. The diet included fruits, vegetables, grains, legumes, and soybean products without caloric restriction. No animal products were allowed except egg white and one cup per day of non-fat milk or yoghurt; 10% of calories as fat, 15-20% protein, and 70-75% carbs. Cholesterol intake was limited to 5 mg/day. Subjects also asked to practice stress management techniques at least 1 hour per day;3 hours exercise per week; smoking cessation (only 1 person was smoking in experimental group at baseline); and twice-weekly group meetings. Control group: no intervention. Asked to follow advice of personal physician.
- Comments: Perhaps one of the most cited studies in support of a the protective effects of a low-fat diet, Cited over 750 times (previous publication cited over 1500) according to Google Scholar, which is unfortunate due to the tremendous amount of co-contaminant interventions. Along with an extremely low fat diet, the experimental group ate more fruits and vegetables, lost 23.9 pounds (control lost no weight), performed relaxation techniques 1 hour each day, exercised at least 3 hours a week, and had group counseling. The control group had none of this. The experimental group contained only 20 subjects (all male), and the experimental group had 15 (12 men and 3 women). At baseline, the mean age was 4 years higher, mean total cholesterol 8% higher and mean LDL 10% higher in control, and mean BMI 3 points higher in experimental group. 11/32 studies cited list Dr. Ornish as an author.
Miettinen et al. (1972). Effect of cholesterol-lowering diet on mortality from coronary heart-disease and other causes. A twelve-year clinical trial in men and women
Outcome: Significant decrease in coronary heart disease (CHD)death in men ( 5.7 deaths /1000 person-years vs 13 deaths /1000 person-years in the control). Non-significant decrease in CHD in women.
- Overview: 12 year non-randomized trial taking place in 2 large mental hospitals. Nikilla hospital (N) was given the experimental diet, while the control group in Kellokoski hospital (K) continued on their typical diet. After 6 years, the diets switched hospitals, with hospital K now receiving the experimental diet.
- Intervention: The experimental diet involved replacing milk fat with soybean oil, replacing butter with soft polyunsaturated margarine, less meat and eggs, and more root vegetables. The control diet remained the same.
- Comments: In hospital N, Blood cholesterol fell 18% in men and 12% in women, indicating they were following the diet. This study received a lot of criticism when it was published due to the fact that it was not randomized, and the physicians were not blinded. Never the less, it remains to be one of the most famous studies ever done on this topic, possibly due to its length and strong results( in men at least).
Paul Leren (1970). The Oslo Diet-Heart Study: Eleven-Year Report (See original clinical trial directly below)
Outcome: After 11 years (3/4 of subjects followed for 10 years), at the P=0.05 level, significant difference between fatal MI between groups. No significant difference in fatal myocardial re-infarctions, fatal heart failure or death preceded by chest pains. No difference in total cardiovascular mortality at the P=0.05 level.
- Overview: Report on subjects enrolled in the 5 year randomized trial in 412 men ages 30-64 recently diagnosed with a myocardial infarction (MI), randomized control diet or cholesterol lowering diet, 11 years after beginning.
- Main Points: No further clinical or laboratory evaluation or dietary advice was given. The surviving subjects in the intervention group were “advised to adhere to the cholesterol lowering diet in the future” while the control group was informed “that reduced fat intake possibly might be beneficial, but received no detailed dietary instructions.”
- Comments: No dietary assessment for 6 years after clinical trial finished. Results are based on the unlikely assumption that subjects continued their diet regimen on their own with no follow up or intervention for 6 years.
Paul Leren (1968). The effect of Plasma-cholesterol lowering diet in male survivors of myocardial infarctions. A controlled clinical trial.
Outcome: Experimental group had significantly less myocardial re-infarctions and acquired angina pectoralis. When stratified by age, the results were significant only in subjects younger than 60. Subjects with more MI’s also had higher cholesterol levels if they were younger than 60. No association between cholesterol levels and sudden death in either age group.
- Overview: 5 year randomized trial in 412 men ages 30-64 recently diagnosed with a myocardial infarction (MI), randomized control diet or cholesterol lowering diet.
- Main Points: Intervention: cholesterol lowering diet low in animal fats and dietary cholesterol, rich in vegetable oils. Cholesterol lowering of 31% was achieved and maintained for entire duration of study
- Comments: Linear relationship between cholesterol levels and relapse rates for subjects under 60 years old. After age 60, there was no difference in the cholesterol levels between those with and without relapses. Results reached significance after 3 years of following the diet. Study suggests long term adherence to diet high in vegetable oils and low in animal fats is beneficial for subjects younger than 60 who have been recently diagnosed with a MI.
Bierenbaum et al. (1967). Modified-Fat Dietary Management of the Young Male With Coronary Disease. A Five-Year Report.
Outcome: The rate of recurrent heart attacks were experimental group: 4,450/100,000 person years in the experimental group Vs. 7,143/100,000 person years in the control. Experimental group had 19 recurrent MIs for 427 person years while control group had 16 recurrent MIs per 224 person years.
- Overview: Non-randomized 5-year clinical trial of 100 male subjects with coronary heart disease matched to a control group with similar characteristics.
- Main Points: Intervention was 1 of 2 diets: Diet 1: 28% calories from fat, 50% mix of corn-safflower oil; Diet 2: 28% calories from fat, 50% mix of coconut-peanut oil; Study groups were given at least 5 prepared meals per week. Control diet: not changed from their normal diet
- Comments: Control group chosen after experimental group. Not-randomized. After 5 years, no significant difference in cholesterol lowering between diet 1 and diet 2. No difference in the cholesterol levels of the survivors or the deceased in the control group. In experimental group, cholesterol levels decreased equally for both survivors and deceased. Final cholesterol levels of experimental vs control group almost identical.
Christakis et al. (1966). Effect of the Anti-Coronary Club program on coronary heart disease risk-factor status.
Outcome: In the active group, there were 8 events out of 2,357 person years, which is an incidence of 339/100,000. In the 8 subjects with diagnosed cardiovascular disease (CVD), 3 died of heart disease. There were 18 total deaths from other causes. In the control group: 12 events occurred out of 1,224 person years, which is an incidence of 980/100,000. Out of the 12 with CVD, all were alive at the end. There were 6 total deaths from other causes.
- Overview: Non-randomized 5-year clinical trial of 814 men ages 40-59 with no prior evidence of heart disease. Events defined as: myocardial infarction (MI), angina with EKG change, angina without EKG change. Experimental group divided into Active experimental group and Inactive experimental group depending on their adherence to study.
- Main Points: Intervention diet: a diet equal in quantities of 3 types of fat: saturated, polyunsaturated, monounsaturated; Beef, mutton, pork limited to 4 meals per week; Butter replaced with margarine and vegetable oil; Ice cream, hard cheese reduced; High levels of fruits and vegetables added to diet. Overweight subjects placed on a 1600 calorie diet to reduce weight.
- Comments: Not randomized. Experimental group further broken up into subjects who followed the protocol and those who didn’t, making the results less valid. Experimental diet consisted of many co-founding factors and interventions, such as increased fruit and vegetable intake and low calorie diets which resulted in weight loss. Control group chosen after experimental group chosen, with half as many subjects.